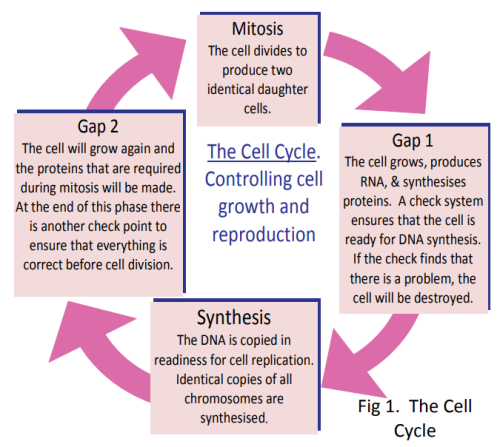
Scientists Douglas Hanahan and Robert Weinberg think that all the different types of cancers share six essential changes in the physiology of the cell. These changes all contribute to the production of a successful tumour. They called these six essential characteristics the Hallmarks of Cancer (Fig. 2).
1. Uncontrolled Growth
Normal cells start or stop growing in response to signals. Cancer cells do not respond to these signals. They will grow when there are no growth signals and continue to grow when they are getting stop signals. So no matter what colour the traffic lights are, cancer cells will go!
2. Evading Death
Normal cells are meant to die when they get old or damaged. Signals in the cell start a process where the cell membrane is disrupted and enzymes break down the cell contents, which are then engulfed by neighbouring cells. This is called programmed cell death or apoptosis. Cancer cells avoid programmed cell death. They have the ability to repress (ignore) the signals that start the process of apoptosis.
3. Angiogenesis
This means that all cells must be in close proximity (within 100µm) of a capillary if they are to survive. Growth of a tumour is not possible past a certain size unless the cells are capable of attracting blood vessels to grow into the tumour in order to supply nutrients and remove wastes. We say a tumour is angiogenic if it has the ability to attract blood vessels to grow into it.
4. Becoming Immortal
Normal cells have a limited number of times that they can divide before they stop growth. Sequences of DNA on the ends of chromosomes called telomeres are responsible for making sure that chromosomes do not fuse end‐to‐end during cell division. Each time a cell divides, the telomeric DNA gets slightly shorter. When it gets so short that it cannot protect the chromosome anymore, the cell dies. In cancer cells the telomeric DNA does not get shorter because an enzyme called telomerase is released that lengthens the telomeres so the cell can keep on replicating endlessly.
5. Invading Other Tissues and Avoiding Detection (Metastasis)
It is common for cancers to move from the site of the primary tumour to other parts of the body. This is called tissue invasion or metastasis. The immune system is constantly on the lookout for cells that are foreign or do not belong. Cancer cells often look different to normal cells and when spreading out will invade tissues different to their own. In order to survive, pre‐cancer cells and cancer cells must evade detection by the immune system.
6. Promoting Mutations
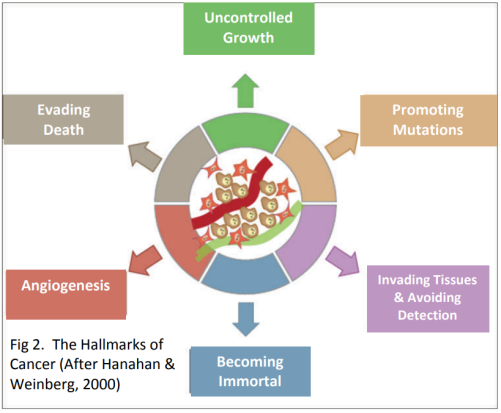
The development of cancer requires an accumulation of mutations in a number of genes over a period of time. Some of these changes accelerate the rate at which mutations occur—meaning that mutations are acquired at a faster rate. Together all these characteristics contribute to the progression of normal cells into cancer (Fig 3).