By studying donated brains from the Brain Bank, Professor Faull’s team have shown that neurons containing γ-aminobutyric acid (GABA), a neurotransmitter that acts as a signalling chemical between neurones, are selectively lost in the striatum of the basal ganglia of humans with HD. Unfortunately, it is not possible to treat patients with GABA because of the effect this treatment would have on the rest of the brain.
While investigating the disease in humans is crucial, the use of animal models has also become an important tool for discovering information about many aspects of HD. These animals (e.g. transgenic mice, fruit flies and nematodes) can be manipulated far more easily than humans, progress more quickly to show the symptoms of HD and have shorter life-spans; therefore these models have a huge advantage over the study of humans as it can speed up the rate of research and information gathering. In addition, the brains of these animals can be accessed early, rather than having to wait until death occurs naturally. Animal models are being used to search for potential drug treatments, with a hope that the outcomes can be translatable to the human disease.
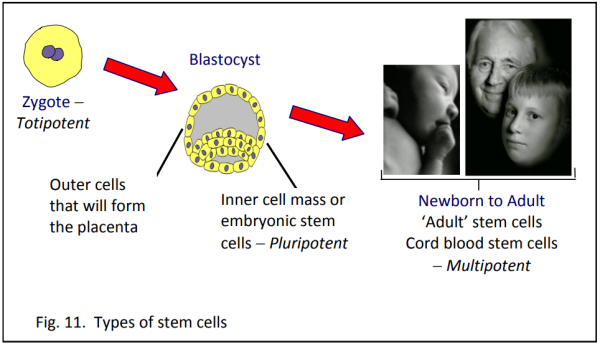
Professor Faull’s team use rats and induce HD by injecting the toxin quinolinic acid into the basal ganglia region of the brain. This toxin is present at higher than normal concentrations in the brains of humans with HD and induces similar symptoms in rats. In addition, the team have transplanted basal ganglia brain cells from a fetal rat into diseased adult rats and found that these cells survive and make new non-diseased GABA-like brain cells. There is hope that the transplantation of fetal brain cells may one day help humans with HD. A similar treatment for Parkinson’s disease has already been trialled in which cells producing the required neurotransmitter dopamine were transferred. Unfortunately the treatment was only partially successful as it resulted in tumour formation in some cases.
While some discoveries in animal models can be directly applied to humans, scientists are always very aware that in many cases this is not possible. Tissue culture studies are another tool to extend our understanding. The cells in tissue culture are isolated – rather than in whole organisms – and investigating these cells in isolation can reduce the ‘noise’ associated with studying the full organism. However, these cells may behave differently when they are isolated from the whole organism, therefore information gathered from isolated cells needs to be further investigated with a view to the whole organism.
While no one tool offers all the answers, it must be kept in mind that all these tools play an important part in extending our understanding of the disease and will eventually enable scientists to finding a cure for HD.